Abstract
Purpose
The investigation examines the impact of a standardized sepsis order set and algorithm utilizing non-invasive monitoring for early-goal directed therapy (EGDT) in an emergency center setting on the clinical outcomes of sepsis in cancer patients.
Methods
Single-center, retrospective study comparing clinical outcomes of sepsis before and after routine usage of a standardized order set and algorithm for non-invasive elements of EGDT for sepsis in an emergency center of a comprehensive cancer center. The outcomes measures evaluated were 28-day in-hospital mortality, intensive care unit length of stay, hospital length of stay, goal mean arterial pressure and urine output within the first 6 h of treatment, time to measurement of lactic acid, and appropriateness and timeliness of initial antibiotic therapy.
Results
The 28-day in-hospital mortality was significantly lower in the post-intervention group compared to the pre-intervention group (20 vs. 38 %, p = 0.005). The percentages of patients who reached their goal mean arterial pressure (74 vs. 90 %, p = 0.004) and goal urine output (79 vs. 96 %, p = 0.002) during the first 6 h of treatment were higher the after than the before group. No significant differences were detected in the rest of the outcome measures.
Conclusions
Implementation of a standardized sepsis order set and algorithm to improve compliance with the non-invasive elements of EGDT for sepsis in cancer patients in the emergency center setting was associated with a decreased 28-day in-hospital mortality rate.
Similar content being viewed by others
Introduction
Sepsis is the tenth leading cause of death in the United States (US) accounting for 1.4 % of all deaths [1]. The annual incidence of sepsis in cancer patients has been estimated at about 1,500 cases per 100,000 cancer patients per year [2, 3], and that in the non-cancer population is around 150 cases per 100,000 patients. Thus, cancer patients are about ten times more likely to develop sepsis [3]. Cancer is not only the most common comorbid condition in sepsis patients with a prevalence of about 17 % [3–5], but it is also the highest risk factor for mortality compared to other comorbid conditions [6].
In 2004, the Surviving Sepsis Campaign (SSC) guidelines recommended the use of early-goal directed therapy (EGDT) based on one large randomized trial [7]. These guidelines were updated in 2008 [8], and were further supported by several subsequent trials that corroborated the benefit of EGDT in severe sepsis and septic shock [9–15]. In addition to the evidence presented in the guidelines, many others have shown improvement in clinical outcomes following the implementation of EGDT [16–19].
Surveys of academic and community emergency departments (EDs) have shown that the majority of EDs do not utilize EGDT [20–22]. The most common reasons for not following the SSC guidelines were lack of resources and specialty monitoring equipment, lack of physician and nursing acceptance, critical shortages in nursing staff, difficulties in recognizing sepsis early, and difficulties with central venous cannulation necessary for some of the invasive elements of EGDT (e.g., measurement of central venous pressure (CVP) and central or mixed venous oxygen saturation) [23–28]. Among these invasive elements of EGDT, CVP has recently been found to not correlate well with intravascular fluid status and not accurately predict the response to a fluid resuscitation [29]. Many experts no longer recommend CVP as a decision making tool to guide fluid resuscitation. Early lactate measurement, which does not require an invasive device, has been proven to accurately classify the severity of illness in patients with severe sepsis and septic shock [30–32]. In hemodynamically stable patients with febrile neutropenia, early lactate elevation was associated with a significant increase in the risk for septic shock within 48 h [33] while early lactate clearance serves as a reliable marker for improvement in global tissue hypoxia. Therefore, measuring lactate may substitute for measuring central venous oxygen saturation [34–36].
Recognizing sepsis is often difficult in cancer patients because of altered presentation of the systemic inflammatory response syndrome (SIRS). For instance, the white blood cell count may be elevated by corticosteroids or growth factors (g-CSF, GM-CSF) or decreased as a result of chemotherapy or malignancy. In addition, frequent use of corticosteroids may mask fever. Whether non-invasive implementation of EGDT can improve clinical outcomes of sepsis in cancer patients has not been studied. We designed an order set and an algorithm for non-invasive implementation of EGDT using serum lactate to substitute for measuring central venous oxygen saturation, and the purpose of this study was to evaluate if implementation of non-invasive EGDT in the EC setting for septic cancer patients was associated with improved clinical outcomes.
Methods
The study was a single-center retrospective cohort design using a historical control group. This study was approved by our hospital’s institutional review board and the need for informed consent was waived.
The goal was to implement a non-invasive sepsis EGDT management protocol in our emergency center (EC). Prior to implementation, formal instructions and briefing were provided to all EC staff. Education on early recognition of the potentially septic patient at triage was emphasized.
A multidisciplinary group of physicians, nurses, respiratory therapists, and pharmacists designed an algorithm to guide the care for a potentially septic patient presenting to our EC. The algorithm focused on early identification at triage based on vital signs, timely laboratory evaluation including point-of-care lactic acid measurement, timely administration of antibiotics and aggressive resuscitation with intravenous normal saline (Fig. 1). Patients whose blood pressure did not normalize or who had an elevated lactic acid level of ≥4 mmol/L were entered into the septic shock arm of the algorithm. Vasopressor therapy consisting of either norepinephrine or dopamine was initiated immediately for MAP < 65 mmHg that persisted after the hydration goal of > 20 mL/kg was achieved.
To emphasize the importance of timely clinical management, a sepsis documentation tool was devised to allow the nurse to record vital signs every 15 min and record input and output hourly until the patient was stable (Fig. 2). At each hourly interval the nurse was prompted to document the communication with the treating physician about the patients’ status.
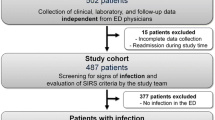
From March 1, 2010 to September 6, 2010, a total of 10,849 patients were admitted for treatment in the EC and 355 required admission to the ICU. During this time, 100 adult (≥18 years of age) cancer patients met the criteria for severe sepsis or septic shock according to the SCC 2008 International Guidelines, which constituted the post-intervention group. The pre-implementation group included the time period of June 1, 2007 through February 1, 2010, where a total of 53,850 patients were admitted for treatment in the EC and 1,432 required admission to the ICU. Of those patients admitted to the ICU, 389 were classified as having sepsis and from this cohort, 100 patients were randomly selected using a random number generator to meet the number needed to achieve adequate power. Retrospective review of this cohort established the historical control. Patients were included in the study if they were admitted from the EC to the intensive care unit (ICU) exhibiting ≥2 signs of SIRS, with suspicion or documentation of infection and either an elevated lactic acid (≥4 mmol/L), multiple organ dysfunction, and/or evidence of hypotension (systolic blood pressure <90 mmHg or MAP ≤ 65 mmHg) after adequate fluid resuscitation (> 20 mL/kg). Patients were excluded from the study if they were pregnant, had pre-existing do not resuscitate orders, or if they arrived to the EC with refractory shock and passed away within 24 h. These patients were “not early” in the course of sepsis and were likely to die regardless of the therapy initiated in the EC; they were not relevant to our investigation of the impact of EGDT.
Patient demographic information and pre-defined outcome measures [e.g., length of stay (LOS)] were recorded. The Charlson comorbidity score was used to compare the impact of cancer type, stage of disease, and comorbidities in both groups [37]. The pre- and post-implementation medical records were reviewed for 28-day in-hospital mortality, adequacy of antibiotics, and attainment of goal blood pressure (MAP > 65 mmHg) and goal urine output (>0.5 ml/kg/h) as categorical variables. Continuous outcome variables were hospital LOS, ICU LOS, time in EC, time to first antibiotic, time to lactic acid level, time to vasopressors, and total fluid administration. Time zero for these measures was defined as the time when the patients arrived in an EC bed. Blood cultures were collected using standardized antisepsis and collection practices as dictated by protocol. A dedicated phlebotomist was assigned to the EC for all shifts, or in emergencies, blood culture collection is done by nursing personnel. Each blood culture consists of an Aerobic Bactec 26 plus and an Isolator 10 lysis centrifugation tube and samples are planted for growth within 4 h. Central line infections were suspected if the intensity of bacteremia of a peripheral blood culture vs. a central line culture was a ratio of 5:1 exists.
Definitions
Patients who were alive at discharge or survived 28 days were considered “alive” for data analysis unless the patient was discharged with comfort measures only and was expected to die at home. An adequate empiric antibiotic regimen was defined as a regimen containing at least one antibiotic with in vitro activity against each of the pathogens causing a particular episode of sepsis administered within 6 h of arrival to the EC bed. Vancomycin is considered as inadequate therapy for methicillin-resistant Staphylococcus aureus (MRSA) if the vancomycin minimum inhibitory concentration (MIC) for that bacterial isolate was ≥2 mcg/mL.
Statistical analysis
The primary a priori outcome measure was 28-day in-hospital mortality. Secondary outcomes included ICU LOS, hospital LOS, attainment of goal MAP and urine output within the first 6 h of EC treatment, time to measurement of lactic acid, and adequacy and timeliness of initial antibiotic therapy. Group sample sizes of 100 each in the before and after groups would achieve 81 % power to detect a 20 % difference in the 28-day in-hospital mortality rates between the before and after groups.
Descriptive statistics were calculated for demographic variables, clinical characteristics, and clinical outcomes for each group. Statistical tests of differences between the before and after treatment groups were performed; for continuous variables we used t tests or Kruskal–Wallis tests depending on the normality of distribution and for proportions and rations we used chi-square and Fisher’s exact tests.
Tests were declared statistically significant if the p value was <0.05. Analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Demographic data are summarized in Table 1. Hematologic malignancy was common in the study group with leukemia patients accounting for 32 % of the population and lymphoma patients accounting for 17 % of the population. Overall, 40 % of the patients were neutropenic, with an absolute neutrophil count of less than 1,000/mm3. The Charlson comorbidity score which has been used in the oncology literature to predict the incidence of mortality was similar between the two groups [37]. The initial MAP at triage was not significantly different between the two groups (68.7 ± 19.0 mmHg vs. 72.6 ± 16.8 mmHg, p = 0.128) nor was the initial lactic acid level (4.1 ± 3.3 mmol/L vs. 3.7 ± 2.4 mmol/L, p = 0.397). Cultures drawn and sent to the microbiology laboratory within 48 h of EC arrival were positive in 113 (57 %) patients. The organisms isolated as well as site of isolation are in Table 2.
Primary and secondary outcomes are reported in Table 3. The 28-day in-hospital mortality was significantly lower in the after group compared to the before group (20 vs. 38 %, p = 0.005). The percentages of patients who reached their goal blood pressure (74 vs. 90 %, p = 0.004) and urine output (79 vs. 96 %, p = 0.002) within the first 6 h of management were significantly better in the after group. The study failed to detect any other significant differences in the other outcome measures. However, there is a clear trend that the ICU LOS may be decreased from 5.1 to 2.5 days (p = 0.067) before and after implementation of our EGDT intervention.
Discussion
The results of this trial indicate that implementation of an order set and algorithm for the treatment of severe sepsis and septic shock using a non-invasive implementation of EGDT is associated with improved 28-day in-hospital mortality. Although it is possible that the use of invasive monitoring devices may have further improved the clinical outcomes over our non-invasive implementation of EGDT, the non-invasive nature of our adaptation may make it feasible for many EDs to start implementing EGDT for sepsis.
Lactic acid has been proven to be a reliable predictor of mortality of sepsis. Elevated serum lactate, (≥ 4 mmol/L) independent of organ failure and failure to clear lactate during early resuscitation are both associated with an increase in mortality [30–36]. In December 2008, we implemented the use of point-of-care arterial blood gas and lactate to improve the time to recognition of patients with decreased tissue perfusion.
Another important principle in the management of severe sepsis and septic shock is to provide adequate initial empiric antimicrobial therapy in a timely manner. Several clinical trials in patients with blood stream infections, ventilator associated pneumonia, and other nosocomial infections have demonstrated improved outcomes, including mortality, when adequate empiric antimicrobial therapy is initiated [38–41]. Delays in the time to effective antibiotic administration were shown to be related to in-hospital mortality in a large multicenter, retrospective cohort. The survival rate for those patients who received antibiotics within 1 h of onset of hypotension was 79.9 % and for each hour after, the rate of survival decreased by about 7.6 % over a total time period of 6 h [42]. In addition to increases in mortality, delays in appropriate antibiotics after the onset of hypotension also increase the incidence of acute kidney injury which is associated with higher mortality [43]. The time to antibiotics in patients who presented to our EC with a MAP < 65 mmHg was not significantly different in either group.
In another retrospective review of critically ill cancer patients, time to administration of antibiotics of >2 h and changes in organ failure between days 1 to 3 were the only two factors that negatively affected 30-day mortality [44]. Based on this information the SSC guidelines now recommend that antibiotics be administered within 1 h after the recognition of severe sepsis and septic shock [8]. Through this trial we were able to determine how well we were complying with the guidelines. While every case was not ideal we are using this information to investigate why there was a delay in administration of antibiotics to prevent delays in the future. Not only is timing of antibiotics important but also adequacy of antibiotics. The most common reasons for inadequacy of antibiotics in this trial were multi-drug resistant gram-negative bacteria (n = 12), MRSA with a vancomycin MIC of ≥2 (n = 6), fungal infection (n = 4), and vancomycin-resistant Enterococcus (n = 1).
Potential limitations of this study include its retrospective nature and the selection of patients who met ICU admission criteria. In terms of the retrospective nature of the study, we can only conclude that the implementation of the standardized order set and algorithm was associated with an improvement in mortality. Direct cause and effect cannot be concluded from this work. A randomized trial would not have been possible in this situation because implementation of the project required education of the entire EC staff making it impossible to have a control group not affected by the concept of EGDT. The time period for patient inclusion differed between the two groups; seasonal differences in the patient population cannot be ruled out. Regarding patient selection, criteria for ICU admission included the presence of persistent hypotension, as well as signs of severe sepsis such as elevated lactic acid levels and organ system failure. This population was of interest to our study because EGDT has been proven to be of most benefit in those patients requiring ICU admission. The original EGDT study by Rivers et al. [7], also only included patients admitted to the ICU. Theoretically by increasing perfusion and oxygenation to tissues, one may prevent further organ damage which could result in better outcomes. The question of whether EGDT in the ED would prevent patients from an ICU admission was not addressed by this study. Another point of discussion is the difficulty in obtaining severity of illness scores, such as SOFA and APACHE II, in a retrospective study. At the time this data was retrospectively collected, there was no reliable documentation of Glasgow Come Score to assess patients baseline SOFA scores and APACHE II scores. However, we were able to collect the Charlson comorbidity score which incorporates type of cancer, presence of metastasis, and additional comorbid conditions. Finally, the study was performed at a single EC of a comprehensive cancer center. Our institution is a tertiary referral center and there is a possibility that the cancer patients we treat with severe sepsis and septic shock may have more progressive disease than a general oncology population; therefore, the conclusions may not be generalizable to other institutions.
Conclusion
Implementation of a standardized sepsis order set and algorithm to improve compliance with the non-invasive elements of EGDT in a cancer patient population was associated with improvement in the 28-day mortality rate and in higher proportions of patients reaching their goal MAP and urine output during the first 6 h of management.
References
Heron M, Hoyert DL, Murphy SL et al (2009) Deaths: final data for 2006. Natl Vital Stat Rep 57(14):1–134
Williams MD, Braun LA, Cooper LM et al (2004) Hospitalized cancer patients with severe sepsis: analysis of incidence, mortality, and associated costs of care. Crit Care 8(5):R291–R298
Danai PA, Moss M, Mannino DM, Martin GS (2006) The epidemiology of sepsis in patients with malignancy. Chest 129(6):1432–1440
Martin GS, Mannino DM, Eaton S et al (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348(16):1546–1554
Alberti C, Brun-Buisson C, Burchardi H et al (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28(2):108–121
Angus DC, Linde-Zwirble WT, Lidicker J et al (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29(7):1303–1310
Rivers E, Nguyen B, Havstad S et al (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19):1368–1377
Dellinger RP, Levy MM, Carlet JM et al (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med 36(1):296–327
Micek ST, Roubinian N, Heuring T et al (2006) Before–after study of a standardized hospital order set for the management of septic shock. Crit Care Med 34(11):2707–2713
Shapiro NI, Howell MD, Talmor D et al (2006) Implementation and outcomes of the multiple urgent sepsis therapies (MUST) protocol. Crit Care Med 34(4):1025–1032
Nguyen HB, Corbett SW, Steele R (2007) Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased morality. Crit Care Med 35(4):1105–1112
Kortgen A, Niederprum P, Bauer M (2006) Implementation of an evidenced-based “standard operating procedure” and outcome in septic shock. Crit Care Med 34(4):943–949
Sebat F, Johnson D, Musthafa AA et al (2005) A multidisciplinary community hospital program for early and rapid resuscitation of shock in nontrauma patients. Chest 127(5):1729–1743
Shorr AF, Micek ST, Jackson WL Jr et al (2007) Economic implications of an evidence-based sepsis protocol: can we improve outcomes and lower costs? Crit Care Med 35(5):1257–1262
Trzeciak S, Dellinger RP, Abate N et al (2006) Translating research to clinical practice: a 1-year experience with implementing early goal-directed therapy for septic shock in the emergency department. Chest 129(2):225–232
Thiel SW, Asghar MF, Micek ST et al (2009) Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis. Crit Care Med 37(3):819–824
Jones AE, Focht A, Horton JM, Kline JA (2007) Prospective external validation of the clinical effectiveness of an emergency department-based early goal-directed therapy protocol for severe sepsis and septic shock. Chest 132(2):425–432
Puskarich MA, Marchick MR, Kline JA et al (2009) One year mortality of patients treated with an emergency department based early goal directed therapy protocol for severe sepsis and septic shock: a before and after study. Crit Care 13(5):R167
Levy MM, Dellinger RP, Townsend SR et al (2010) The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med 38:367–374
Casserly B, Baram M, Walsh P et al (2011) Implementing a collaborative protocol in a sepsis intervention program: lesion learned. Lung 189:11–19
De Miguel-Yanes JM, Andueza-Lillo JA, Gonzalez-Ramallo VJ (2006) Failure to implement evidence-based clinical guidelines for sepsis at the ED. Am J Emerg Med 24(5):553–559
Cronshaw HL, Daniels R, Bleetman A et al (2011) Impact of the Surviving Sepsis Campaign on the recognition and management of severe sepsis in the emergency department: are we failing? Emerg Med J 28:670–675
Jones AE, Kline JA (2005) Use of goal-directed therapy for severe sepsis and septic shock in academic emergency departments. Crit Care Med 33(8):1888–1889
Nguyen HB, Oh J, Otero RM et al (2010) Standardization of severe sepsis management: a survey of methodologies in academic and community settings. J Emerg Med 38(2):122–130
Carlbom DJ, Rubenfeld GD (2007) Barriers to implementing protocol-based sepsis resuscitation in the emergency department—results of a national survey. Crit Care Med 35:2525–2532
Lyon RM, McNally SJ, Hawkins M et al (2010) Early goal-directed therapy: can the emergency department deliver? Emerg Med J 27:355–358
O’Neill R, Morales J, Jule M. Early goal-directed therapy for severe sepsis/septic shock: which components of treatment are more difficult to implement in a community-based emergency department? J Emerg Med 2012 doi:10.1016/j.jemermed.2011.03.024
Mikkelsen ME, Gaieski DF, Goyal M et al (2010) Factors associated with nonadherence to early-goal directed therapy in the ED. Chest 138(3):551–558
Marik PE, Baram M, Vahid B (2008) Does the central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 134:172–178
Shapiro NI, Howell MD, Talmor D et al (2005) Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med 45(5):524–528
Trzeciak S, Dellinger RP, Chansky ME et al (2007) Serum lactate as a predictor of mortality in patients with infection. Intensive Care Med 33(6):970–977
Mikkelsen ME, Miltiades AN, Gaieski DF et al (2009) Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med 37(5):1670–1677
Mato AR, Luger SM, Heitjan et al (2010) Elevation in serum lactate at the time of febrile neutropenia in hemodynamically-stable patients with hematologic malignancies is associated with the development of septic shock within 48 hours. Cancer Biol Ther 9(8):585–589
Jones AE, Shapiro NI, Trzeciak S et al (2010) Lactate clearance vs. central venous oxygen saturation as goals of early sepsis therapy. JAMA 303(8):739–746
Nguyen HB, Rivers EP, Knoblich BP et al (2004) Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 32(8):1637–1642
Arnold RC, Shapiro NI, Jones AE et al (2009) Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock 32(1):35–39
Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S (2004) An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer 4:94
Ibrahim EH, Sherman G, Ward S et al (2000) The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 118(1):146–155
Leibovici L, Shraga I, Drucker M et al (1998) The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med 244(5):379–386
Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH (2002) Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest 122(1):262–268
Kollef MH, Ward S, Sherman G et al (2000) Inadequate treatment of nosocomial infections is associated with certain empiric antibiotic choices. Crit Care Med 28(10):3456–3464
Kumar A, Roberts D, Wood KE, Light B et al (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinate of survival in human septic shock. Crit Care Med 34(6):1589–1596
Bagshaw SM, Lapinsky S, Dial S, Arabi Y et al (2009) Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med 35(5):871–881
Larche J, Azoulay E, Fieux F, Mesnard L et al (2003) Improved survival of critically ill cancer patients with septic shock. Intensive Care Med 29(10):1688–1695
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hanzelka, K.M., Yeung, SC.J., Chisholm, G. et al. Implementation of modified early-goal directed therapy for sepsis in the emergency center of a comprehensive cancer center. Support Care Cancer 21, 727–734 (2013). https://doi.org/10.1007/s00520-012-1572-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1572-y