ABSTRACT
Background
Providers consistently underutilize professional interpreters in healthcare settings even when they perceive benefits to using professional interpreters and when professional interpreters are readily available. Little is known about providers’ decision-making processes that shape their use of interpreters.
Objective
To understand the variety of considerations and parameters that influence providers’ decisions regarding interpreters.
Design
A qualitative, semi-structured interview guide was used to explore providers’ decision making about interpreter use. The author conducted 8 specialty-specific focus groups and 14 individual interviews, each lasting 60–90 minutes.
Participants
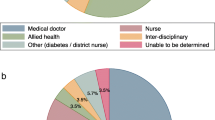
Thirty-nine healthcare professionals were recruited from five specialties (i.e., nursing, mental health, emergency medicine, oncology, and obstetrics-gynecology) in a large academic medical center characterized as having “excellent” interpreter services.
Approach
Audio-recorded interviews and focus groups were transcribed and analyzed using grounded theory to develop a theoretical framework for providers’ decision-making processes.
Key Results
Four factors influence providers’ choice of interpreters: (a) time constraints, (b) alliances of care, (c) therapeutic objectives, and (d) organizational-level considerations. The findings highlight (a) providers’ calculated use of interpreters and interpreting modalities, (b) the complexity of the functions and impacts of time in providers’ decision-making process, and (c) the importance of organizational structures and support for appropriate and effective interpreter utilization.
Conclusions
Providers actively engage in calculated use of professional interpreters, employing specific factors in their decision-making processes. Providers’ understanding of time is complex and multidimensional, including concerns about disruptions to their schedules, overburdening others’ workloads, and clinical urgency of patient condition, among others. When providers make specific choices due to time pressure, they are influenced by interpersonal, organizational, therapeutic, and ethical considerations. Organizational resources and guidelines need to be consistent with institutional policies and professional norms; otherwise, providers risk making flawed assessments about the effective and appropriate use of interpreters in bilingual health care.
Similar content being viewed by others
REFERENCES
Hsieh E. Understanding medical interpreters: reconceptualizing bilingual health communication. Health Commun. 2006;20:177–86.
Schenker Y, Pérez-Stable EJ, Nickleach D, Karliner LS. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011;26:712–7.
Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved. 2008;19:352–62.
Lee KC, Winickoff JP, Kim MK, et al. Resident physicians’ use of professional and nonprofessional interpreters: a national survey. J Am Med Assoc. 2006;296:1050–3.
Ginde AA, Sullivan AF, Corel B, Caceres JA, Camargo CA Jr. Reevaluation of the effect of mandatory interpreter legislation on use of professional interpreters for ED patients with language barriers. Patient Educ Couns. 2010;81:204–6.
Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24:256–62.
Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–54.
Hsieh E, Ju H, Kong H. Dimensions of trust: the tensions and challenges in provider-interpreter trust. Qual Health Res. 2010;20:170–81.
Butow PN, Goldstein D, Bell ML, et al. Interpretation in consultations with immigrant patients with cancer: how accurate is it? J Clin Oncol. 2011;29:2801–7.
Green J, Free C, Bhavnani V, Newman T. Translators and mediators: bilingual young people’s accounts of their interpreting work in health care. Soc Sci Med. 2005;60:2097–110.
Leanza Y, Boivin I, Rosenberg E. Interruptions and resistance: a comparison of medical consultations with family and trained interpreters. Soc Sci Med. 2010;70:1888–95.
Angelelli CV. A professional ideology in the making: bilingual youngsters interpreting for their communities and the notion of (no) choice. Transl Interpretation Stud. 2010;5:94–108.
Hsieh E. “I am not a robot!” Interpreters’ views of their roles in health care settings. Qual Health Res. 2008;18:1367–83.
Rosenberg E, Seller R, Leanza Y. Through interpreters’ eyes: comparing roles of professional and family interpreters. Patient Educ Couns. 2008;70:87–93.
Moreno MR, Otero-Sabogal R, Newman J. Assessing dual-role staff-interpreter linguistic competency in an integrated healthcare system. J Gen Intern Med. 2007;22:S331–5.
Wros P. Giving voice: incorporating the wisdom of Hispanic RNs into practice. J Cult Divers. 2009;16:151–7.
Locatis C, Williamson D, Gould-Kabler C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25:345–50.
Cunningham H, Cushman LF, Akuete-Penn C, Meyer DD. Satisfaction with telephonic interpreters in pediatric care. J Natl Med Assoc. 2008;100:429–34.
Nápoles AM, Santoyo-Olsson J, Karliner LS, O’Brien H, Gregorich SE, Pérez-Stable EJ. Clinician ratings of interpreter mediated visits in underserved primary care settings with ad hoc, in-person professional, and video conferencing modes. J Health Care Poor Underserved. 2010;21:301–17.
Hsieh E, Hong SJ. Not all are desired: providers’ views on interpreters’ emotional support for patients. Patient Educ Couns. 2010;81:192–7.
Meischke H, Chavez D, Bradley S, Rea T, Eisenberg M. Emergency communications with limited-English-proficiency populations. Prehosp Emerg Care. 2010;14:265–71.
Price EL, Perez-Stable EJ, Nickleach D, Lopez M, Karliner LS. Interpreter perspectives of in-person, telephonic, and videoconferencing medical interpretation in clinical encounters. Patient Educ Couns. 2012;87:226–32.
Garcia EA, Roy LC, Okada PJ, Perkins SD, Wiebe RA. A comparison of the influence of hospital-trained, ad hoc, and telephone interpreters on perceived satisfaction of limited English-proficient parents presenting to a pediatric emergency department. Pediatr Emerg Care. 2004;20:373–8.
U.S. Census Bureau. Selected social characteristics in the United States: 2008–2012 American Community Survey 5-year estimates. 2014. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_5YR_DP02. Accessed April 19 2014.
IQ Solutions. Naitonal standards for culturally and linguistically appropriate services. In: USDoHaH, ed. Services. Washington, DC: U.S. Department of Health and Human Services; 2001.
Hsieh E. Interpreters as co-diagnosticians: overlapping roles and services between providers and interpreters. Soc Sci Med. 2007;64:924–37.
Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 2nd ed. Thousand Oaks, CA: Sage; 1998.
Charmaz K. Constructing a Grounded Theory: A Practical Guide Through Qualitative Analysis. New York: Sage; 2006.
Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: Sage; 2006.
Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. Thousand Oaks, CA: Sage; 2013.
Irish DP, Lundquist KF, Nelsen VJ, eds. Ethnic Variations in Dying, Death, and Grief: Diversity in Universality. New York: Routledge; 1993.
Tuckett AG. Truth-telling in clinical practice and the arguments for and against: a review of the literature. Nurs Ethics. 2004;11:500–13.
Diamond LC, Tuot D, Karliner L. The use of Spanish language skills by physicians and nurses: policy implications for teaching and testing. J Gen Intern Med. 2012;27:117–23.
Cohen S, Moran-Ellis J, Smaje C. Children as informal interpreters in GP consultations: pragmatics and ideology. Soc Health Illn. 1999;21:163–86.
Mazor SS, Hampers LC, Chande VT, Krug SE. Teaching Spanish to pediatric emergency physicians: effects on patient satisfaction. Arch Pediatr Adolesc Med. 2002;156:693–5.
Parsons JA, Baker NA, Smith-Gorvie T, Hudak PL. To ‘Get by’ or ‘get help’? A qualitative study of physicians’ challenges and dilemmas when patients have limited English proficiency. BMJ Open. 2014;4.
Cowden JD, Thompson DA, Ellzey J, Artman M. Getting past getting by: training culturally and linguistically competent bilingual physicians. J Pediatr. 2012;160:891–2.e1.
Splevins KA, Cohen K, Joseph S, Murray C, Bowley J. Vicarious posttraumatic growth among interpreters. Qual Health Res. 2010;20:1705–16.
Yang C-F, Gray B. Bilingual medical students as interpreters–what are the benefits and risks? N Z Med J. 2008;121:15–28.
Crossman KL, Wiener E, Roosevelt G, Bajaj L, Hampers LC. Interpreters: telephonic, in-person interpretation and bilingual providers. Pediatrics. 2010;125:e631–8.
Kuo DZ, O’Connor KG, Flores G, Minkovitz CS. Pediatricians’ use of language services for families with limited English proficiency. Pediatrics. 2007;119:e920–7.
Diamond LC, Wilson-Stronks A, Jacobs EA. Do hospitals measure up to the national culturally and linguistically appropriate services standards? Med Care. 2010;48:1080–7.
Lambert SD, Loiselle CG. Combining individual interviews and focus groups to enhance data richness. J Adv Nurs. 2008;62:228–37.
Fagan MJ, Diaz JA, Reinert SE, Sciamanna CN, Fagan DM. Impact of interpretation method on clinic visit length. J Gen Intern Med. 2003;18:634–8.
Tocher TM, Larson EB. Do physicians spend more time with non-English-speaking patients? J Gen Intern Med. 1999;14:303–9.
Seale C, Rivas C, Kelly M. The challenge of communication in interpreted consultations in diabetes care: a mixed methods study. Br J Gen Pract. 2013;63:e125–33.
Schouten BC, Schinkel S. Turkish migrant GP patients’ expression of emotional cues and concerns in encounters with and without informal interpreters. Patient Educ Couns. in press.
Jacobs EA, Leos GS, Rathouz PJ, Fu P Jr. Shared networks of interpreter services, at relatively low cost, can help providers serve patients with limited English skills. Health Aff (Millwood). 2011;30:1930–8.
Kazzi GB, Cooper C. Barriers to the use of interpreters in emergency room paediatric consultations. J Paediatr Child Health. 2003;39:259–63.
O’Leary SCB, Federico S, Hampers LC. The truth about language barriers: one residency program’s experience. Pediatrics. 2003;111:e569–73.
Jacobs EA, Diamond LC, Stevak L. The importance of teaching clinicians when and how to work with interpreters. Patient Educ Couns. 2010;78:149–53.
Contributors
The author gratefully acknowledges her research team members: Haiying Kong, MA, and Hyejung Ju, Ph.D., for their passion and hard work for data collection and analysis and Michelle Farabough, MA, for her preliminary data analysis as a graduate course project. Finally, I thank Dr. Eric Kramer for his continuous feedback throughout all phases of the research project.
Funders
The author gratefully acknowledges the support of Grant #1R03MH76205-01-A1 (Title: Providers’ Views of the Roles of Medical Interpreters) funded by National Institutes of Health/National Institute of Mental Health (NIMH).
Prior Presentations
2012 National Communication Association Convention, November 18, 2012.
Conflicts of Interest
The author declares that she does not have any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsieh, E. Not Just “Getting by”: Factors Influencing Providers’ Choice of Interpreters. J GEN INTERN MED 30, 75–82 (2015). https://doi.org/10.1007/s11606-014-3066-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-3066-8