Abstract
To determine whether ketamine use for tracheal intubation, compared to other sedative use, is associated with a lower risk of post-intubation hypotension in hemodynamically-unstable patients in the emergency department (ED), we analyzed the data of a prospective, multicenter, observational study—the second Japanese Emergency Airway Network (JEAN-2) Study—from February 2012 through November 2017. The current analysis included adult non-cardiac-arrest ED patients with a pre-intubation shock index of ≥0.9. The primary exposure was ketamine use as a sedative for intubation, with midazolam or propofol use as the reference. The primary outcome was post-intubation hypotension. A total of 977 patients was included in the current analysis. Overall, 24% of patients developed post-intubation hypotension. The ketamine group had a lower risk of post-intubation hypotension compared to the reference group (15% vs 29%, unadjusted odds ratio [OR] 0.45 [95% CI 0.31–0.66] p < 0.001). This association remained significant in the multivariable analysis (adjusted OR 0.43 [95% CI 0.28–0.64] p < 0.001). Likewise, in the propensity-score matching analysis, the patients with ketamine use also had a significantly lower risk of post-intubation hypotension (OR 0.47 [95% CI, 0.31–0.71] P < 0.001). Our observations support ketamine use as a safe sedative agent for intubation in hemodynamically-unstable patients in the ED.
Similar content being viewed by others
Introduction
Tracheal intubation for hemodynamically-unstable patients is a critical resuscitation procedure in the emergency department (ED). Yet, the literature has documented that the adverse event rate in ED patients who underwent airway management remains high—e.g., 22% with post-intubation hypotension and up to 4% with cardiac arrest1,2. Building strong evidence base for intubation medications (e.g., sedative agents) is critical for the development of optimal intubation strategies in hemodynamically-unstable patients (e.g., patients with pre-intubation hypotension and shock) who are at high risk for these clinically-important adverse events3.
Ketamine—a sympathomimetic agent that releases catecholamines and inhibits their reuptake4 —has been recommended for patients at high risk for hypotension and cardiac arrest5, albeit the limited evidence. Within the sparse literature, a randomized controlled trial of 80 operating room patients has demonstrated that ketamine increased the mean arterial pressure by 10% during induction6. In contrast, other small-scale studies (n ≤ 112) have also reported that ketamine use was associated with blunted hypertensive responses and post-intubation hypotension in hemodynamically-unstable patients7,8. Despite the clinical importance, there remains a controversy over the relationship of ketamine use with the risk of post-intubation hypotension in the ED.
To address the knowledge gap in the literature, we analyzed the data from a large multicenter prospective study to determine the association of ketamine use—compared with midazolam or propofol use—with the risk of post-intubation hypotension in hemodynamically-unstable ED patients.
Results
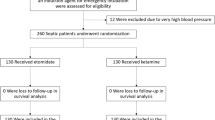
During the 46-month study period, the second Japanese Emergency Airway Network (JEAN-2) recorded a total of 7,657 patients with emergency airway management in the 15 EDs (capture rate, 97%; Supplemental Fig. 1). We excluded 3,183 patients with cardiac arrest, 169 children (aged <18 years), 2,361 patients with a shock index (SI) of <0.9, 511 patients without sedative use, 50 patients intubated with other sedatives, 18 patients intubated with multiple sedatives, and 388 patients with missing data. The remaining 977 patients were eligible for the current analysis. Overall, the median age was 67 years (interquartile range, 53–78 years) and 68% were male. Ketamine was used in 316 patients (32%). The baseline characteristics of the ketamine and reference groups are summarized in Table 1. The ketamine group was more likely to be intubated for shock (53%) and by an emergency medicine resident, compared to the reference group (both P < 0.05).
Overall, the incidence of post-intubation hypotension (i.e., systolic blood pressure [SBP] of ≤90 mmHg or ≥20% decrease in SBP) was 23%. The ketamine use was associated with a significantly lower risk of post-intubation hypotension compared with the reference group (15% vs. 27%; unadjusted odds ratio [OR], 0.45; 95% CI, 0.31–0.66; P < 0.001; Table 2). This association remained significant in the multivariable model adjusting for potential confounders (adjusted OR, 0.43; 95% CI, 0.29–0.65; P < 0.001; Fig. 1).
The association of ketamine use of post-intubation hypotension in unadjusted and adjusted models, and propensity score matched analysis. Compared with the reference group, ketamine use was significantly associated with a lower risk of post-intubation hypotension in both unadjusted and adjusted models. This association was consistent in the propensity score matching analysis.
In the sensitivity analysis, using one-to-one propensity score matching, the baseline characteristics of 286 matched pairs were successfully balanced between the ketamine and reference groups (all standardized differences of <10; Supplemental Table 1). Similar to the primary analysis, the patients with ketamine use had a significantly lower risk of post-intubation hypotension, compared to the patients in the reference group (16% vs. 28%), with a corresponding OR of 0.47 (95% CI, 0.31–0.71; P < 0.001; Fig. 1). In the analysis stratified by SI (dichotomized by the median SI), the probability of post-intubation hypotension was 24% (95% CI, 21–28%) in patients with a SI 0.90–1.12 and 21% (95% CI, 17–26%) in patients with a SI ≥ 1.13. In both groups, ketamine use was significantly associated with a lower risk of post-intubation hypotension compared with the reference group (adjusted odds ratio [aOR], 0.39 [95% CI, 0.23–0.65] in patients with a SI of 0.90–1.12; aOR 0.42 [95% CI, 0.23–0.76] in patients with a SI ≥ 1.13). Likewise, in the multivariable model including SI (as a continuous variable) and product term of ketamine use–X–SI, both SI and product term were not significantly associated with the risk of post-intubation hypotension, indicating that the effect of ketamine use on the risk of post-intubation hypotension does not differ by the degree of pre-intubation hemodynamic stability.
Discussion
In this analysis of 977 adult hemodynamically-unstable patients who underwent intubation in the ED, we found that ketamine use as a sedative agent was associated with a significantly lower risk of post-intubation hypotension, compared with the reference group. This association remained significant across the use of different statistical assumptions—e.g., the analyses of multivariable hierarchical model and PS-matched model. To the best of our knowledge, this is the first study that has investigated the association between ketamine use and the risk of post-intubation hypotension in ED population.
These findings are consistent with the previous non-emergency-medicine literature that has reported the benefit of ketamine use for intubation. For example, a single-center randomized control trial of 80 patients in the operative room setting, White et al. have reported that thiopental decreased the mean arterial pressure by 11%, whereas ketamine increased the mean arterial pressure by 10%6. By contrast, several studies have also shown that the use of ketamine was associated with a higher risk of post-intubation hypotension in hemodynamically-unstable patients7,8. For example, a single-center descriptive study of 12 critically-ill operating room patients has reported that six patients had a decreased ventricular contractility and four patients had decreases in cardiac output or mean arterial blood pressure after ketamine use7. In addition, in an observational study of 120 out-of-hospital patients managed by a single emergency medical service, the patients with a high SI (≥0.9) had not only a blunted sympathetic response but also higher risk of post-intubation hypotension compared to patients with a low SI (<0.9)8. The reasons of these discrepancies between the studies might be attributable to the difference of study design (e.g., examination of the effect of ketamine according to SI), sample (e.g., differences in the proportion of the elderly), and study settings (e.g., operative room, out-of-hospital, and ED settings)4,7,8,9, or any combination of these factors. Nevertheless, the validity of our findings is buttressed by the use of data from a multi-ED prospective study with high quality data (e.g., 97% capture rate) with a sample size that is many times larger than any other prior studies in this topic as well as rigorous adjustment for potential confounding.
The underlying mechanisms of the favorable effect of ketamine on hemodynamically-unstable patients are likely multifactorial. In addition to its amnestic, analgesic, and bronchodilation properties, ketamine also releases catecholamines and increases norepinephrine levels by inhibiting their neuronal and extraneuronal reuptake, thereby increasing heart rate, cardiac output, and arterial pressure4. Dowdy et al. demonstrated that the cardio-stimulatory effects were attributable to enhanced norepinephrine release secondary to depressed baroreceptor reflex activity10. In addition, the literature has also suggested that the use of midazolam and propofol is associated with a higher risk of post-intubation hypotension11. Consequently, our findings may be explained, at least partially, by the combination of these potential mechanisms.
According to the World Health Organizations Report, ketamine is the most commonly-used anesthetic agents in the developing countries because ketamine is readily available and inexpensive12. While etomidate is frequently used for intubation in industrialized countries (e.g., North America), etomidate is not approved in many developing countries and some industrialized countries (e.g., Japan). A previous randomized controlled study comparing ketamine and etomidate in out-of-hospital and ED patients showed no significant difference in the severity of organ dysfunction and mortality after intubation13. In addition, while some controversy persists regarding the use of ketamine for rapid sequence intubation in patients with multisystem trauma at risk for both hypotension and elevated intracranial pressure14, the evidence to refute its use is not robust. Indeed, studies have indicated that ketamine does not interfere with cerebral metabolism, reduce regional glucose metabolism, or increase oxygen consumption but may benefit patients with a neurologic injury by a catecholamine-mediated increase in arterial pressure and cerebral perfusion15,16,17,18. Building on the currently-available evidence, our findings lend another significant support to the use ketamine for hemodynamically-unstable patients in the ED, particularly where etomidate is not available or approved for intubation19.
The present study has several potential limitations. First, the data do not include information on post-ED outcomes, such as in-hospital mortality. While post-intubation hypotension might be considered as a transient adverse event, the literature has documented that the post-intubation hypotension in the ED is a risk factor for higher in-hospital mortality and longer hospital length of stay1,20. Second, there may have been be a self-reporting bias, which may lead to an underestimation of the proportion of post-intubation hypotension. However, we used the previously applied standardized protocol with structured data forms and high capture rate21,22,23,24,25 and the incidence of post-intubation hypotension in our study was consistent to that was reported in a previous systematic review26. Third, despite the rigorous adjustment, the causal inference (i.e., the contribution of ketamine use to the risk of post-intubation hypotension) may have been confounded by unmeasured factors, such as infusion volume, vasopressor use, and comorbid illnesses (e.g., heart failure). Yet, the multivariable model adjusting for the primary indication and PS-matching addressed, at least partially, such unmeasured confounding. Lastly, our study sample chiefly consisted of patients in the academic EDs in Japan and hence our inferences may not be generalized in different practice settings. While it is tempting to dismiss the broader applicability of these findings, these are pharmacologically and clinically plausible, and are likely present in different clinical settings4,5,7.
Based on the analysis of data from a large prospective multicenter study of ED airway management, we found that the use of ketamine was associated with a significantly lower risk of post-intubation hypotension, compared to the use of midazolam or propofol, in hemodynamically-unstable ED patients. The significant association persisted across the different statistical assumptions. As post-intubation hypotension is an important risk factor of unfavorable post-ED outcomes1,20, for clinicians, our observations lend significant support to the use of ketamine as a sedative for rapid sequence intubation in hemodynamically-unstable patients. For researchers, our data should advance the research into the development of optimal airway management strategies, which will, in turn, improve outcomes in critically-ill patients in the ED.
Methods
Study design and setting
This is an analysis of the data from a multicenter prospective observational study of consecutive ED patients who underwent emergency airway management— JEAN-2 registry from February 2012 through November 2016. The study design, setting, methods of data collection, and measured variables have been reported elsewhere21,22,23,24,25,27,28. In brief, the JEAN-2 study is a consortium of 15 academic and community medical centers from different geographic regions across Japan. The participating institutions were certified as 12 level I and three level II equivalent trauma centers. These EDs had a median of 27,000 patient visits in the ED per year (range, 14,000–65,000). All institutions were affiliated with emergency medicine residency training programs and staffed by emergency medicine attending physicians. Transitional-year residents (postgraduate-years 1 and 2) also rotated through the ED and participated in intubations. Each ED maintained individual protocols about the policy and procedures for ED intubations. Intubations were performed by resident physicians or attending physicians at the discretion of attending physicians. The study was approved by the institutional review board of each participating hospital with waiver of informed consent.
Selection of participants
In the present study, we selected all adult non-cardiac-arrest patients (aged ≥18 years) who underwent intubation in the ED with a pre-intubation SI of ≥0.9, as a marker of hemodynamic instability8. SI of ≥0.9 better represents hemodynamical instability compared with SBP alone8. We excluded (1) patients who received no sedatives, (2) patients who received sedatives other than ketamine, propofol, or midazolam (i.e., diazepam and thiopental that were used for 7% of patients with any sedative use in the study)23, (3) patients who received two or more types of sedatives, and (4) patients with missing data on age, weight, SBP or heart rate at pre-intubation, SBP at post-intubation, sedative, intubation device, or specialty of intubator.
Data collection and processing
Immediately after each intubation encounter, the intubator completed a standardized data collection form that included the patient demographics (e.g., age, sex), weight and height, primary indication for the intubation, methods of intubation, all medications and devises used to facilitate airway management, level of training and specialty of the intubator, number of attempts, success or failure, associated adverse events, and vital signs (heart rate, blood pressure, arterial oxygen saturation) measured immediately before, immediately after, and 30 minutes after the intubation19,21,22,23,24,25,27,28,29,30. The JEMNet (Japanese Emergency Medicine Network) coordinating center and site investigator at each ED monitored compliance with data form completion. Where the data form was missing, it was returned to the intubator for completion. If information on the data form contained contradiction, the investigator interviewed the intubator for airway management detail. These post hoc interviews occurred within fourteen days of the patient encounter. An intubation “attempt” was defined by a single insertion of the laryngoscope (or other device) past the teeth. An attempt was recognized as success if tracheal tube was placed through the vocal cords and confirmed by a quantitative or colorimetric end-tidal carbon dioxide monitor.
Primary exposure
The primary exposure of interest was ketamine use for emergency airway management, compared with midazolam or propofol use as the reference.
Outcome measure
The outcome measure of interest was post-intubation hypotension, defined as SBP of ≤90 mmHg during the 30-minute period following intubation or ≥20% decrease in SBP between pre-intubation and immediately after intubation3,19,24,29,31.
Statistical analysis
For the purpose of the present analysis, we categorized the patients into the ketamine and reference (i.e., midazolam or propofol use) groups. To investigate the association between the use of ketamine and the risk of post-intubation hypotension, we constructed unadjusted and adjusted two-level hierarchical models with a binomial response using random intercepts for the EDs to account for patient clustering within the ED. In the multivariable analysis, we adjusted for age, sex, body mass index (BMI), primary indication, premedication use, paralytic use, and intubator’s specialty. These covariates were chosen based on the clinical plausibility and a priori knowledge19,27,29,32,33. BMI was classified into three categories (<18.5, 18.5–24.9, and ≥25.0 kg/m2)27. Primary indication for intubation was classified into four categories: respiratory failure, medical shock, traumatic indication, and others (e.g., airway obstruction, altered mental status, other medical indications)33. Specialty of the intubator was categorized into transitional-year resident, emergency medicine resident, emergency attending physician, and other specialties.
In the sensitivity analysis to determine the robustness of our inference, we also performed a propensity matching (PS) analyses. First, we computed the PS by fitting a logistic regression model that estimates the probability of ketamine use conditional on the covariates in the primary multivariable model above. Second, we conducted one-to-one matching of patients between the ketamine and reference groups with the closest estimated PS within a caliper (≤0.20 of the pooled standard deviation of estimated logits) using the nearest neighbor method without replacement34. We computed the standard differences to examine the appropriate matching of the baseline characteristics between the two groups. A standard difference of >10% was regarded as imbalanced. Lastly, in the PS-matched patients, we conducted a logistic regression analysis to examine the association between ketamine use and risks of post-intubation hypotension.
To determine whether the effect of ketamine use on the risk of post-intubation hypotension differs by the degree of pre-intubation hemodynamic stability, we conducted two additional analyses. First, we stratified the patients into two groups according to the median SI: (1) patients with a SI of 0.90–1.12 and (2) patients with a SI of ≥1.13. Then, we fit the multivariable model for each group. Second, we also fit a multivariable model including a product term of ketamine use–X–SI. P < 0.05 was considered statistically significant. Analyses were performed with the use of STATA 14.1 (StataCorp, College Station, TX) and JMP 12.2.0 (SAS Institute, Inc., Cary, NC).
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to no IRB’s approval of data sharing but are available from the corresponding author on reasonable request.
Change history
05 February 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Heffner, A. C., Swords, D., Kline, J. A. & Jones, A. E. The frequency and significance of postintubation hypotension during emergency airway management. J. Crit. Care 27(417), e419–413 (2012).
Heffner, A. C., Swords, D. S., Neale, M. N. & Jones, A. E. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation 84, 1500–1504 (2013).
Smischney, N. J. et al. Incidence of and Risk Factors For Post-Intubation Hypotension in the Critically Ill. Med. Sci. Monit. 22, 346–355 (2016).
Lippmann, M., Appel, P. L., Mok, M. S. & Shoemaker, W. C. Sequential cardiorespiratory patterns of anesthetic induction with ketamine in critically ill patients. Crit. Care Med. 11, 730–734 (1983).
Morris, C., Perris, A., Klein, J. & Mahoney, P. Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent? Anaesthesia 64, 532–539 (2009).
White, P. F. Comparative Evaluation of Intravenous Agents for Rapid Sequence Induction—Thiopental, Ketamine, and Midazolam. Anesthesiology 57, 279–285 (1982).
Waxman, K., Shoemaker, W. C. & Lippmann, M. Cardiovascular effects of anesthetic induction with ketamine. Anesth. Analg. 59, 355–358 (1980).
Miller, M. et al. Hemodynamic Response After Rapid Sequence Induction With Ketamine in Out-of-Hospital Patients at Risk of Shock as Defined by the Shock Index. Ann. Emerg. Med. 68, 181–188 e182 (2016).
Kakazu, C., Lippmann, M. & Hsu, D. Ketamine: a positive-negative anaesthetic agent. Br. J. Anaesth. 117, 267 (2016).
Dowdy, E. G. & Kaya, K. Studies of the mechanism of cardiovascular responses to CI-581. Anesthesiology 29, 931–943 (1968).
Hawkins, E., Moy, H. P. & Brice, J. H. Critical airway skills and procedures. Emerg. Med. Clin. North Am. 31, 1–28 (2013).
Ketamine Critical Care Report 2012. Expert Committee on Drug Dependence. World Health Organization, https://www.who.int/medicines/areas/quality_safety/4.2Ketamine_criticalreview.pdf?ua=1 (2012).
Jabre, P. et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet 374, 293–300 (2009).
Wyte, S. R., Shapiro, H. M., Turner, P. & Harris, A. B. Ketamine-induced intracranial hypertension. Anesthesiology 36, 174–176 (1972).
Langsjo, J. W. et al. Effects of subanesthetic doses of ketamine on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology 99, 614–623 (2003).
Himmelseher, S. & Durieux, M. E. Revising a dogma: ketamine for patients with neurological injury? Anesth. Analg. 101, 524–534, table of contents (2005).
Cohen, L. et al. The effect of ketamine on intracranial and cerebral perfusion pressure and health outcomes: a systematic review. Ann. Emerg. Med. 65, 43–51 e42 (2015).
Hudetz, J. A. & Pagel, P. S. Neuroprotection by ketamine: a review of the experimental and clinical evidence. J. Cardiothorac. Vasc. Anesth. 24, 131–142 (2010).
Hasegawa, K. et al. Increased incidence of hypotension in elderly patients who underwent emergency airway management: an analysis of a multi-centre prospective observational study. Int. J. Emerg. Med. 6, 12 (2013).
Heffner, A. C., Swords, D. S., Nussbaum, M. L., Kline, J. A. & Jones, A. E. Predictors of the complication of postintubation hypotension during emergency airway management. J. Crit. Care 27, 587–593 (2012).
Hagiwara, Y. et al. Prospective validation of the modified LEMON criteria to predict difficult intubation in the ED. Am. J. Emerg. Med. 33, 1492–1496 (2015).
Goto, T. et al. Multiple failed intubation attempts are associated with decreased success rates on the first rescue intubation in the emergency department: a retrospective analysis of multicentre observational data. Scand. J. Trauma Resusc. Emerg. Med. 23, 5 (2015).
Goto, Y. et al. Techniques and outcomes of emergency airway management in Japan: An analysis of two multicentre prospective observational studies, 2010–2016. Resuscitation 114, 14–20 (2017).
Takahashi, J. et al. Association of fentanyl use in rapid sequence intubation with post-intubation hypotension. Am. J. Emerg. Med. 36, 2044–2049 (2018).
Goto, T. et al. Factors Associated with First-Pass Success in Pediatric Intubation in the Emergency Department. West. J. Emerg. Med. 17, 129–134 (2016).
Green, R. et al. Incidence of postintubation hemodynamic instability associated with emergent intubations performed outside the operating room: a systematic review. Cjem 16, 69–79 (2015).
Yakushiji, H. et al. Associations of obesity with tracheal intubation success on first attempt and adverse events in the emergency department: An analysis of the multicenter prospective observational study in Japan. PLoS One 13, e0195938 (2018).
Okamoto, H. et al. Comparison of video laryngoscopy versus direct laryngoscopy for intubation in emergency department patients with cardiac arrest: A multicentre study. Resuscitation 136, 70–77 (2018).
Hasegawa, K. et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann. Emerg. Med. 60, 749–754 e742 (2012).
Nakao, S., Kimura, A., Hagiwara, Y. & Hasegawa, K., Japanese Emergency Medicine Network, I. Trauma airway management in emergency departments: a multicentre, prospective, observational study in Japan. BMJ Open 5, e006623 (2015).
Walls, R. M., Brown, C. A. 3rd., Bair, A. E. & Pallin, D. J., Investigators, N. I. Emergency airway management: a multi-center report of 8937 emergency department intubations. J. Emerg. Med. 41, 347–354 (2011).
Reich, D. L. et al. Predictors of hypotension after induction of general anesthesia. Anesth. Analg. 101, 622–628, table of contents (2005).
Franklin, C., Samuel, J. & Hu, T. C. Life-Threatening Hypotension Associated With Emergency lntubation and the Initiation of Mechanical Ventilation. Am J Emrg Med 12, 425–428 (1994).
Austin, P. C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res 46, 399–424 (2011).
Acknowledgements
The authors acknowledge the JEAN-2 investigators for their contributions to this project. We also thank our many emergency physicians and residents for their perseverance in pursuing new knowledge about this vital resuscitative procedure.
Author information
Authors and Affiliations
Consortia
Contributions
T.I. takes responsibility for the paper as a whole. T.I., T.G., J.T., and K.H. conceived the study. T.G., H.O., Y.H., H.W., and K.H. supervised the conduct of the study. T.G., H.O., J.T., and K.H. provided statistical advice. T.I. and T.G. analyzed the data. T.I. drafted the manuscript, and all authors contributed substantially to its revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A comprehensive list of consortium members appears at the end of the paper
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishimaru, T., Goto, T., Takahashi, J. et al. Association of ketamine use with lower risks of post-intubation hypotension in hemodynamically-unstable patients in the emergency department. Sci Rep 9, 17230 (2019). https://doi.org/10.1038/s41598-019-53360-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-53360-6
This article is cited by
-
Positive effects of low-dose S-ketamine on preventing myocardial injury after thoracoscopic lobectomy in patients aged 70 to 85
BMC Anesthesiology (2024)
-
The Physiologically Difficult Airway and Management Considerations
Current Anesthesiology Reports (2024)
-
Ketamine Use in the Intubation of Critically Ill Children with Neurological Indications: A Multicenter Retrospective Analysis
Neurocritical Care (2024)
-
Clinical outcomes after a single induction dose of etomidate versus ketamine for emergency department sepsis intubation: a randomized controlled trial
Scientific Reports (2023)
-
A specialized airway management team for COVID-19 patients: a retrospective study of the experience of two Canadian hospitals in Toronto
Canadian Journal of Anesthesia/Journal canadien d'anesthésie (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.